Extradural hematoma
This refers to collection of blood in between the skull and dura mater.
More commonly seen in younger patients (children, adolescence)
Extradural hematoma is always associated with skull fractures, most frequently, the temporal bone. (since pterion is the thinnest part of skull, involvement of this area causes tearing of the middle meningeal artery)
Of course, involvement of the posterior fossa and frontal bone is also possible.
However, the hematoma is not always arterial in origin, it may be due to a tear to the dural venous sinuses as well.
Classical presentation of extradural hematoma is : (<1/3 of the cases)
Lucid interval, where after initial injury, patient is conscious, alert, oriented, and only complaints of headache. Minutes or hours later, the condition worsens, with deterioration of consciousness, contralateral hemiparesis/plegia, and ipsilateral pupillary dilatation.
Early diagnosis and treatment of subdural hematoma is VITAL.
CT brain is confirmatory, where it'll appears as a lentiform, biconvex, or lense-shaped hyperdense mass in between the skull and brain, with or without midline shift.
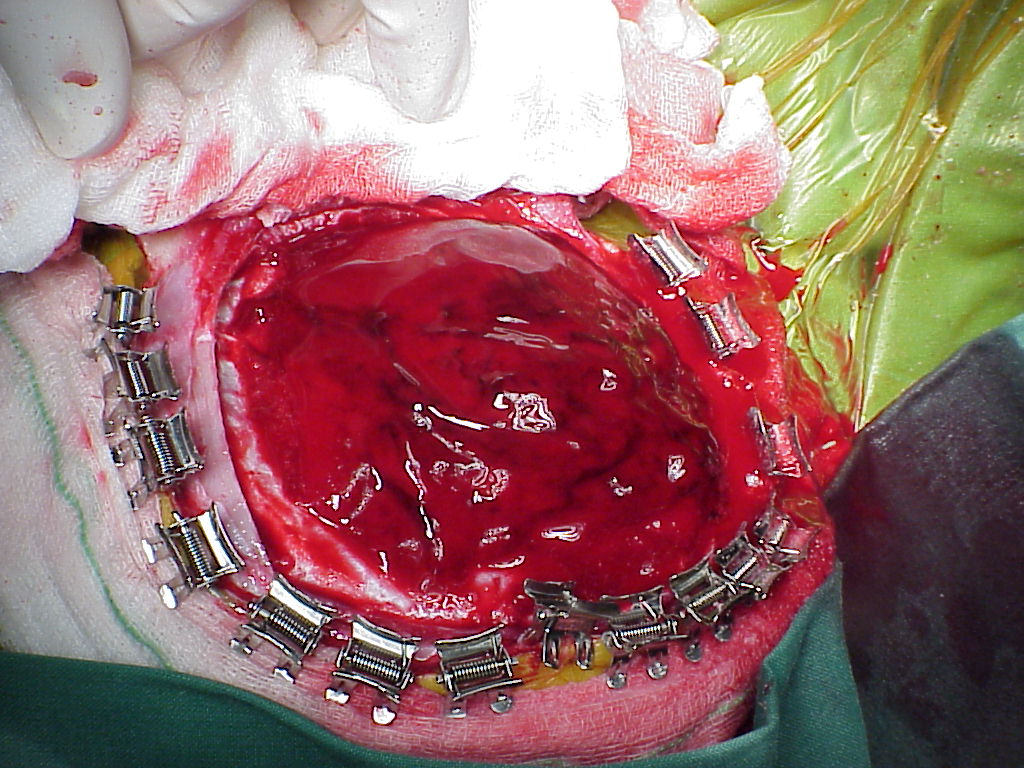
After diagnosis is confirmed, surgical evacuation of the hematoma is required, where craniotomy is performed.
Acute subdural hematoma (ASH)
This is actually more common, with poorer prognosis, higher mortality rate as compared to extradural hematoma.
It refers to blood collection in between the dura and arachnoid mater.
ASH is almost always associated with a primary brain injury.
Most of the time at presentation, the patient has impaired consciousness, which rapidly deteriorates depending on the size of the hematoma.
Again, CT brain is diagnostic.
It'll appears as a crescent shaped, more diffuse (with concavity towards the brain), hyperdense mass in between the brain and skull.
Treatment - surgical evacuation by craniotomy
Chronic subdural hematoma (CSH)
CSH often seen in elderly patients, who is on anti-platelets or anti-coagulants. It is believed to be due to tearing of the bridging veins, which causes formation of clinically inapparent, small ASH. Later, as it breaks down and the volume expands, it becomes symptommatic.
Mostly, patients presents with headache, focal neurological deficit, impaired cognition, seizures, etc (hence, one of the d/d of CVA)
CT brain intepretation :
Acute blood (0-10 days) = hyperdense
Subacute blood (10 days - 2 weeks) = isodense
Chronic blood (>2weeks) = hypodense
Treatment = creating a blurr hole and evacuate the hematoma


No comments:
Post a Comment