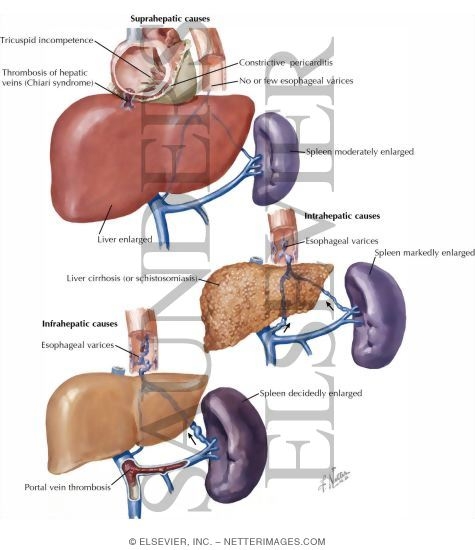
Anatomy of the portal system :
The portal vein is formed behind the neck of pancreas, at the level of L2, by the superior mesenteric and splenic veins.
It ascends up along the free edge of lesser omentum, behind the common bile duct.
It enters the liver by dividing into two of it's tributaries.
The left and right gastric veins joins to it.
The inferior mesenteric veins drains into the splenic veins.
Portal vein is valveless and hence, if there's a raised in pressure in between the right heart and the splanchnic circulation, portal pressure elevates.
The portal vein carries about 1.5L of blood per minute, originating from :
Small bowel (superior mesenteric vein)
Large bowel (inferior mesenteric vein)
Spleen (Splenic vein)
Gastric vein
Pathophysiology
Normal portal pressure is about 5-10mmHg.
Portal hypertension occurs when the portal pressure elevates beyond 12mmHg.
At this point, the collaterals at sites of porto-systemic anastomosis opens up in order to decompress the elevated pressure in the portal system.
As the portal pressure elevates above 20mmHg, there's a risk of the friable, submucosal esophageal varices to rupture, causing massive hematemesis.
Sites of porto-systemic anastomosis :
1) Between left and short gastric veins (portal) and azygous veins (systemic) at the lower esophagus and stomach
2) Caput medusae : Paraumbilical veins (systemic) and vein within the ligamentum teres (portal)
3) Lower rectum : Superior and middle haemorrhoidal veins (portal) and inferior haemorrhoidal veins (systemic)
4) Perihepatic veins of Sappey : Subdiagphramatic veins (portal) and Veins at the upper surface of right liver lobe (systemic)
5) Retroperitoneal veins of Retzius : Retroperitoneal veins (systemic) and Superior + Inferior mesenteric veins (portal)
Causes :
a) Pre-hepatic Causes :
Portal vein thrombosis - seen in umbilical sepsis (infants)
Splenic vein thrombosis - Complication of pancreatitis, pancreatic tumour
b) Intrahepatic Causes :
i) Pre-sinusoidal :
Schistosomiasis
Primary biliary cirrhosis
Chronic active hepatitis
Sarcoidosis
ii) Sinusoidal :
Cirrhosis
Cytotoxic drugs
Vitamin A intoxication
iii) Post-sinusoidal :
Cirrhosis
Veno-occlusive diseases
c) Post-hepatic causes :
Budd-Chiari's syndrome
Tricuspid regurgitation
Constrictive Pericarditis
Clinical presentation (History and Examination)
Malnutrition
Ascites
Hematemesis and Malena
Encephalopathy
Caput medusae
Splenomegaly
Venous hum heard
Look for signs and symptoms of chronic liver disease
How do you manage these patients?
1) Esophageal varices without prior h/o of bleeding
Medical management is ideal in such cases.
Start Propanolol orally to reduce portal pressure, provided that there's no contraindication against B-blockers.
If contraindication present, isosorbide-5-mononitrate is an alternative.
Studies have shown that B-blockers reduces 45% of the risk of bleeding.
2) Ruptured esophageal varices presented with hematemesis
95% of the cases - originating from the esophageal varices, 5% - gastric origin
First, assess the rate and volume of bleeding :
Take pulse and BP in standing and sitting position
Gain IV ascess - Blood is withdrawn for hematocrit, coagulation profile, LFT and BUSE, blood grouping and cross matching
Provide immediate fluid resuscitation (Crystalloids, colloids, or even blood transfusion)
Insert CVP line - for ease of rapid transfusion later to prevent volume overload
Start Vasopressin IV (Contraindicated in angina) or Somastostatin IV.
Or Octreotide IV (more potent and duration of action is longer)
Usually 3 days later, as the patient's condition has stabilised, start B-blocker to reduce portal pressure and prevent further bleeding.
Plan for endoscopic treatment :
a) Band ligation
b) Sclerotherapy (Sodium Tetradecyl Sulphate - STS)
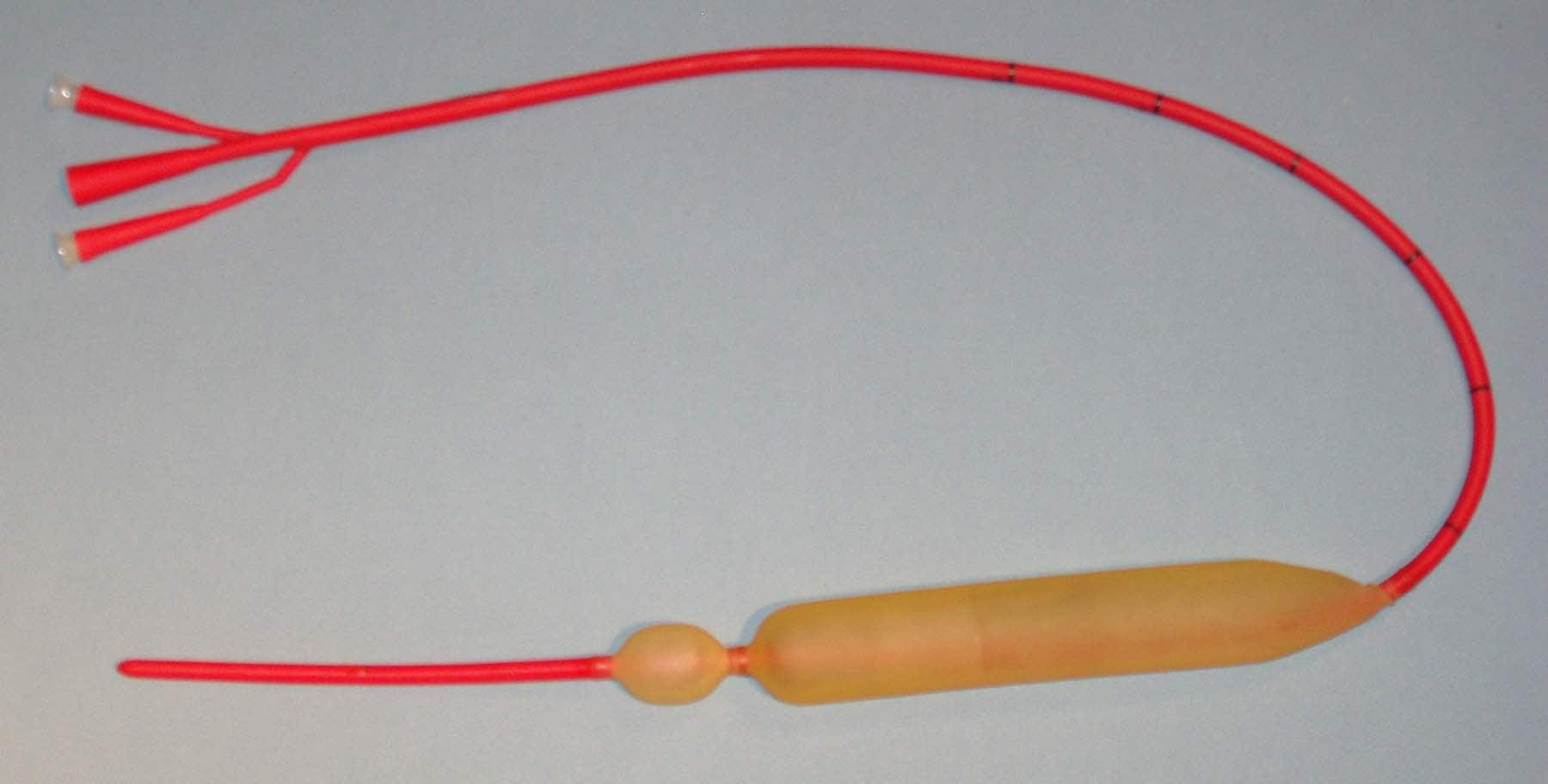
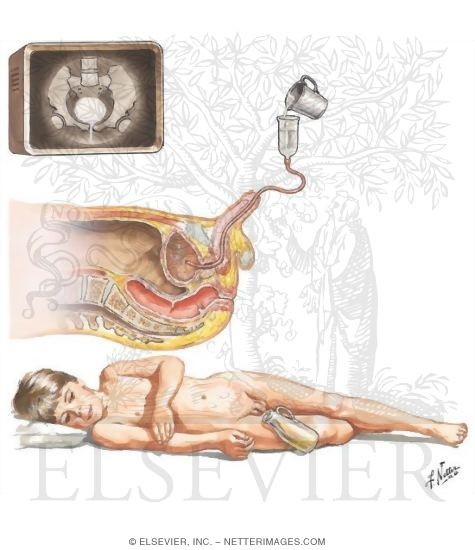
If the patient is not reponsive to the above measures and still bleeding or endoscopic intervention is not available (district hospitals), a Sangstaken-Blakemore tube can be inserted to prevent bleeding to buy time for deciding what's the next step. (Shoiuld be removed after 48 hrs)
Start oral neomycin (to reduce bowel flora -> less conversion of nitrogenous waste within bowel back to ammonia -> prevent hyperammonemia)
Start lactulose (to reduce bowel transit time)
Repeat every 2 weeks the sclerotherapy/band ligation until all the varices have been treated.
Monday, November 23, 2009
Sunday, November 22, 2009
Rectal bleeding
Rectal bleeding usually indicates lower GI bleeding (below duodenojejunal junction). Bear in mind that any patient, aged >45 yrs old, with complaints of :
colickly abdominal pain, PR bleeding and changes in bowel habits
Colorectal CA must be considered unless proven otherwise.
Some causes of rectal bleeding
1) Anal cause
a) Haemorrhoids
Piles are very common.
Uncomplicated piles are not painful.
b) Fissure-in-ano
Fissure-in-ano usually causes painful defecation.
The precipitating cause is usually constipation, hence constipation is usually worsened by the patient fear of passing motion, since it's painful.
Pain usually persists for minutes or even hours after defecation.
c) Carcinoma
The history of anal carcinoma is similar to that of Fissure-in-ano.
However, it's usually seen in the elderly.
d) Trauma
History of penetrating injury into the anus.
Sexual abuse? Anal intercourse?
2) Colorectal causes
a) Carcinoma
As mentioned in previous posts
b) Polyps
The history given by patient is usually the same as carcinoma
c) Diverticulitis
The difference between Diverticulitis and Carcinoma :
Duration : Diverticulitis = longer, Carcinoma = shorter
Pain : Diverticulitis = usually painful, Carcinoma = painless (initial)
Bleeding pattern : Diverticulitis = periodic, massive
Carcinoma = usually smaller in amount, persistent
Mass per abdomen : Diverticulitis = tender, Carcinoma = tenderless
Abdominal radiograph : Diverticulitis = diffuse changes, Carcinoma = localised
d) Inflammatory bowel disease
Usually presented as sudden onset of watery diarrhoea, together with brown stools, mucous, and blood. Ulcerative proctitis can presents as tenesmus
e) Ischaemic colitis, angiodysplasia
f) Irradiative colitis
Especially common in patients with pelvic malignancies, due to irradiation
g) Rectal prolapse
Patient usually complaints of something hanging out at his/her back opening besides PR bleeding
3) Small bowel
a) Meckel's diverticulum
Consider this diagnosis in young adults with frequent painless PR bleeding
b) Acute mesenteric infarction
Patient with h/o of cardiac disease (embolism), with complaints of diffuse abdominal pain, PR bleeding, collapse, with signs of shock, etc -> consider this as well
4) Massive Upper GI bleeding
Due to the massive nature of the upper GI bleeding, the intestinal transit is fast, and hence instead of presenting with hematemesis, patient presents with massive PR bleeding, with shock-like features
5) Bleeding disorders
6) Drugs (anticoagulants)
7) Uremic bleeding
8) Infective causes - dysentry
colickly abdominal pain, PR bleeding and changes in bowel habits
Colorectal CA must be considered unless proven otherwise.
Some causes of rectal bleeding
1) Anal cause
a) Haemorrhoids
Piles are very common.
Uncomplicated piles are not painful.
b) Fissure-in-ano
Fissure-in-ano usually causes painful defecation.
The precipitating cause is usually constipation, hence constipation is usually worsened by the patient fear of passing motion, since it's painful.
Pain usually persists for minutes or even hours after defecation.
c) Carcinoma
The history of anal carcinoma is similar to that of Fissure-in-ano.
However, it's usually seen in the elderly.
d) Trauma
History of penetrating injury into the anus.
Sexual abuse? Anal intercourse?
2) Colorectal causes
a) Carcinoma
As mentioned in previous posts
b) Polyps
The history given by patient is usually the same as carcinoma
c) Diverticulitis
The difference between Diverticulitis and Carcinoma :
Duration : Diverticulitis = longer, Carcinoma = shorter
Pain : Diverticulitis = usually painful, Carcinoma = painless (initial)
Bleeding pattern : Diverticulitis = periodic, massive
Carcinoma = usually smaller in amount, persistent
Mass per abdomen : Diverticulitis = tender, Carcinoma = tenderless
Abdominal radiograph : Diverticulitis = diffuse changes, Carcinoma = localised
d) Inflammatory bowel disease
Usually presented as sudden onset of watery diarrhoea, together with brown stools, mucous, and blood. Ulcerative proctitis can presents as tenesmus
e) Ischaemic colitis, angiodysplasia
f) Irradiative colitis
Especially common in patients with pelvic malignancies, due to irradiation
g) Rectal prolapse
Patient usually complaints of something hanging out at his/her back opening besides PR bleeding
3) Small bowel
a) Meckel's diverticulum
Consider this diagnosis in young adults with frequent painless PR bleeding
b) Acute mesenteric infarction
Patient with h/o of cardiac disease (embolism), with complaints of diffuse abdominal pain, PR bleeding, collapse, with signs of shock, etc -> consider this as well
4) Massive Upper GI bleeding
Due to the massive nature of the upper GI bleeding, the intestinal transit is fast, and hence instead of presenting with hematemesis, patient presents with massive PR bleeding, with shock-like features
5) Bleeding disorders
6) Drugs (anticoagulants)
7) Uremic bleeding
8) Infective causes - dysentry
An approach to a case of Hematemesis
Hematemesis means vomiting of blood.
It can be either a frank blood, or altered, coffee-ground coloured blood (altered by digestive enzyme)
The aetiology of hematemesis is usually proximal to the duodenojejunal junction.
Causes
1) Swallowed blood
Due to hemoptysis, epitaxis
2) Oesophageal causes
Ruptured oesophageal varices
Reflux oesophagitis
Esophageal carcinoma
3) Stomach and duodenum
Peptic ulcer disease
Mallory-Weiss disease
Acute gastric erosions
Gastric carcinoma
4) Bleeding disorders
Hemophilia
Thrombocytopoenia
Coagulopathy (due to liver disease)
5) Drugs
NSAIDS
Aspirin
Steroids
Anticoagulants
6) Others
Uremia
Connective tissue disorders
History : Important questions
1) Is there any h/o of epitaxis, hemoptysis?
2) Ask for h/o of chronic liver disease
3) Any retrosternal burning chest pain radiating upwards or heartburn?
4) Any h/o of dysphagia, odynophagia, weight lost?
5) Ask for h/o of peptic ulcer disease
6) Any h/o of consumption of large meal and alcohol?
7) Does the hematemesis preceded by severe bouts of vomiting?
8) Ask for h/o of anaemia
9) Any recent h/o of acute pancreatitis? Any head injuries? (Cushing's ulcer) Or Any h/o of burns? (Curling's ulcer)
10) Any h/o of bleeding disorders? In the family, is there any?
11) Any h/o of drug intake?
12) Ask for symptoms of uraemia
On examination
1) Depends on the severity of bleeding, does the patients appears to be in shock?
Cool extremities
Prolonged capillary filling time
Tachycardia
Hypotension
Reduced skin turgosity
Altered sensorium
Sunken eyeballs
Dry tongue
Reduced urine output
2) Check around the nose - is there any blood?
3) Examine the chest for any cause of hemoptysis
4) Look for pallor
5) Look for signs of chronic liver disease
6) Any epigastric mass, palpable Left SC nodes?
7) Any epigastric tenderness?
8) Any bruises? Any signs of uremia?
Investigations
1) Full blood count, ESR
Hb level, platelet count, any raised ESR? (connective tissue disorders)
2) Liver function test
3) Coagulation profile (PT and INR)
4) BUSE (Renal profile)
5) Oesophagogastroduodenoscopy (OGD)
It can be either a frank blood, or altered, coffee-ground coloured blood (altered by digestive enzyme)
The aetiology of hematemesis is usually proximal to the duodenojejunal junction.
Causes
1) Swallowed blood
Due to hemoptysis, epitaxis
2) Oesophageal causes
Ruptured oesophageal varices
Reflux oesophagitis
Esophageal carcinoma
3) Stomach and duodenum
Peptic ulcer disease
Mallory-Weiss disease
Acute gastric erosions
Gastric carcinoma
4) Bleeding disorders
Hemophilia
Thrombocytopoenia
Coagulopathy (due to liver disease)
5) Drugs
NSAIDS
Aspirin
Steroids
Anticoagulants
6) Others
Uremia
Connective tissue disorders
History : Important questions
1) Is there any h/o of epitaxis, hemoptysis?
2) Ask for h/o of chronic liver disease
3) Any retrosternal burning chest pain radiating upwards or heartburn?
4) Any h/o of dysphagia, odynophagia, weight lost?
5) Ask for h/o of peptic ulcer disease
6) Any h/o of consumption of large meal and alcohol?
7) Does the hematemesis preceded by severe bouts of vomiting?
8) Ask for h/o of anaemia
9) Any recent h/o of acute pancreatitis? Any head injuries? (Cushing's ulcer) Or Any h/o of burns? (Curling's ulcer)
10) Any h/o of bleeding disorders? In the family, is there any?
11) Any h/o of drug intake?
12) Ask for symptoms of uraemia
On examination
1) Depends on the severity of bleeding, does the patients appears to be in shock?
Cool extremities
Prolonged capillary filling time
Tachycardia
Hypotension
Reduced skin turgosity
Altered sensorium
Sunken eyeballs
Dry tongue
Reduced urine output
2) Check around the nose - is there any blood?
3) Examine the chest for any cause of hemoptysis
4) Look for pallor
5) Look for signs of chronic liver disease
6) Any epigastric mass, palpable Left SC nodes?
7) Any epigastric tenderness?
8) Any bruises? Any signs of uremia?
Investigations
1) Full blood count, ESR
Hb level, platelet count, any raised ESR? (connective tissue disorders)
2) Liver function test
3) Coagulation profile (PT and INR)
4) BUSE (Renal profile)
5) Oesophagogastroduodenoscopy (OGD)
Saturday, November 21, 2009
Short cases - Lumps
1) Dermoid cyst
Dermoid cyst is a cyst located deep to the skin and lined by the skin.
It forms either due to accident during antenatal development or even following injury, some skin is being implanted into the subcutaneous tissue.
Hence, dermoid cyst can be congenital or accquired.
a) Congenital dermoid cyst
History
May be noticed at birth, or years later when it gradually distends to a noticable size. The common complaints, usually by the parents is cosmetic disfigurement since it's a swelling at the neck and face. Rarely it becomes large enough to cause mechanical disability or affecting the vision.
On examination
Congenital dermoid cyst is usually formed when the skin dermatome fuses.
It's commonly found at the midline trunk, face and neck, outer or inner aspect of eye brow, or behind the ear.
Shape is usually spherical, with diameter of 1-2cm.
Smooth surfaced.
Congenital dermoid cyst over the face is usually soft.
Since it usually doesn't contain clear fluid as it supposed to be (mixture of sebum, sweat and desquamated epithelial cells), it doesn't transilluminate.
It fluctuates and if it's large enough, there's fluid thrill as well.
Skin over the cyst is pinchable.
Non-pulsatile, non-compressible, non-reducible.
Local lymph nodes are not enlarged.
b) Accquired implantational dermoid cyst
History
There's history of old injury, such as deep cut, stab injuries and etc.
These implantational dermoid cyst is usually found over areas susceptible to repeated traumas, eg the fingers.
Hence, it can be painful, or even interferes with gripping and touch.
Examination
Seen over sites liable to repeated trauma - beneath skin of fingers.
Size and shape - Spherical, small with diameter 0.5-1cm
Smoothed surace
Due to it's small size, it's almost impossible to elicit specific signs for cystic swelling, which is fluctuation and fluid thrill.
It's usually hard, and the skin overlying it is usually scarred.
The skin is either tethered deep to the scar or within it.
It's mobile over the deeper structures, which is usually normal.
Commonly confused with sebaceous cyst, but with an old scar and h/o of injury is significant for diagnosis.
2) Subcutaneous Abscess

Dermoid cyst is a cyst located deep to the skin and lined by the skin.
It forms either due to accident during antenatal development or even following injury, some skin is being implanted into the subcutaneous tissue.
Hence, dermoid cyst can be congenital or accquired.
a) Congenital dermoid cyst
History
May be noticed at birth, or years later when it gradually distends to a noticable size. The common complaints, usually by the parents is cosmetic disfigurement since it's a swelling at the neck and face. Rarely it becomes large enough to cause mechanical disability or affecting the vision.
On examination
Congenital dermoid cyst is usually formed when the skin dermatome fuses.
It's commonly found at the midline trunk, face and neck, outer or inner aspect of eye brow, or behind the ear.
Shape is usually spherical, with diameter of 1-2cm.
Smooth surfaced.
Congenital dermoid cyst over the face is usually soft.
Since it usually doesn't contain clear fluid as it supposed to be (mixture of sebum, sweat and desquamated epithelial cells), it doesn't transilluminate.
It fluctuates and if it's large enough, there's fluid thrill as well.
Skin over the cyst is pinchable.
Non-pulsatile, non-compressible, non-reducible.
Local lymph nodes are not enlarged.
b) Accquired implantational dermoid cyst
History
There's history of old injury, such as deep cut, stab injuries and etc.
These implantational dermoid cyst is usually found over areas susceptible to repeated traumas, eg the fingers.
Hence, it can be painful, or even interferes with gripping and touch.
Examination
Seen over sites liable to repeated trauma - beneath skin of fingers.
Size and shape - Spherical, small with diameter 0.5-1cm
Smoothed surace
Due to it's small size, it's almost impossible to elicit specific signs for cystic swelling, which is fluctuation and fluid thrill.
It's usually hard, and the skin overlying it is usually scarred.
The skin is either tethered deep to the scar or within it.
It's mobile over the deeper structures, which is usually normal.
Commonly confused with sebaceous cyst, but with an old scar and h/o of injury is significant for diagnosis.
2) Subcutaneous Abscess
History
Throbbing pain which steadily worsens, and keeps patient awaken at night.
Patient usually notice a swelling at the site of pain.
May complaints of fever with chills and rigor.
It may rupture and discharging pus out of the skin before they seek medical attention.
The patient may have h/o of diabetes, having debilitating diseases, or even IV drug use.
Examination
Since the buttocks and upper thigh are usual sites of injection, abscess may be formed there. And in IV drug users, over cubital fossa or groin.
Skin over swelling appears red and shinny.
Surface is not definate.
Usually started as a patch of induration, which later as pus collects, a spherical mass is formed.
There's local rise in temperature.
The edge is not palpable since due to the induration and the edema usually fuses with the normal tissue.
It's tender.
Initially it feels hard, when pus started to collect, it becomes soft at the centre and fluctuates.
Skin over swelling is not pinchable.
Regional lymph nodes may be enlarged and tender
3) Sebaceous cyst
Our skin is kept oily and soft by secretions of sebum from sebaceous gland.
The mouth of the sebaceous glands are located at the hair follicles.
Any blockage over these mouth can result in it's distension within it's own secretion and results in formation of sebaceous cyst.
History
Rarely present before adolescence, since it's a slow-growing swelling.
Usually seen in young adults or middle-aged individual.
It's usually detected incidentally by patients as they're combing their hair, when they complained of scratched lump.
It can be infected, where the size suddenly increased rapidly.
Sebum secreted from wide punctum can be later hardened to form a sebaceous horn.
Examination
It's usually present at scalp, back, shoulders, and scrotum. (Never in the palm and soles since there's no sebaceous gland over these areas)
Skin over swelling is normal unless infected.
Shape - spherical, with smooth surface.
Temperature is not raised and is not tender unless it gets infected.
Edge is easily felt, well-defined.
Consistency - hard.
No fluctuations or fluid thrill.
As the swelling increases in size, the point of fixation will be drawn inwards and punctum is formed. Punctum is diagnostic for sebaceous cyst, but however, only one-half of such swelling presents with a punctum.
Skin over swelling is not pinchable.
Local lymph nodes are not palpable.
4) Lipoma
History
Lipoma is a slow-growing swelling, rarely regresses.
Occurs at any age, but relatively uncommon in children.
Not associated with any symptoms, but presents to the doctor usually because they have noticed a lump and wanted to know what it is.
Patients can have multiple lipoma (lipomatosis), usually over the neck and buttocks.
Examination
Common sites of lipoma includes the upper and lower limb, back, buttocks, neck, etc.
Size is variable, shape - hemiovoid, spherical, etc.
On inspection, surface appears smooth. But when the swelling is palpated carefully, especially when firm pressure is applied, it's lobulated and depression in between these lobulations is seen.
Edge is soft, compressible and tends to slip away from examining hands (slip sign)
Composition - solid fat (fat in body temperature is solid instead of fluid)
Consistency - soft
There's pseudofluctuation, since it's consistency is soft. However, one will notice that on gentle pressure,the plane of swelling over palpating fingers are not tense or not buldging out.
There may be pseudo-transillumination.
Skin over swelling is pinchable.
As muscle is tensed, it may either be more prominent or less (it can arise above or beneath the muscle)
Compressible swelling.
No enlargement of regional lymph nodes.
History taking and examination of a swelling
Some key questions to be asked regarding a swelling (generally)
1. When do you first notice the lump?
REMEMBER, first noticed the lump 3 months ago is not the same as first appeared 3 months ago.
2. How do you notice it?
Below are the 3 commonest answers :
a) It's painful
b) I noticed it accidentally
c) Others told me about it
Generally, if the lump is painful, the commonest aetiology is inflammation.
Most of the patients thought that only painful lumps are cancerous.
3. How does the lump disturbs you?
Basically, the question is asking about the associated symptoms.
It can be pain, discharge, dysphagia, dyspnoea, cosmetically disfiguring, fear of malignancy, etc.
4. Any changes to the lump since you first notice it?
The commonest change is the size.
Whether the lump has increased or decreased in size, or it's size fluctuates.
5. Has the lump ever dissapears before?
Does the lump dissapears when the patient is lying down supine?
or any other activities
6. Do you ever had any other lumps before this?
Asking for multiplicity
7. What do you think is the cause?
Particularly important if there's history of trauma
On examination :
Note the -
a) Position
b) Colour and texture of skin over swelling
c) Size
d) Shape
e) Surface
f) Temperature
g) Tenderness
h) Edge - indistinct/well-defined
i) Composition
Calcified tissues/bone makes the swelling hard
Swelling packed with cells : Firm
Or it might contain fluid (lymph, blood, pus)
Intravascular blood
Gas
j) Consistency
Stony hard - not indentable at all, as hard as bone
Firm - hard, but not as hard as bone
Rubbery - slightly indentable, feels like rubber
Spongy - indentable, but with some resillence
Soft - Squashable, no resillence
k) Fluctuation
Palpate the swelling over 3 planes.
Pressure over the 3rd plane of the swelling usually causes the other 2 planes to buldge out or tensed-up
Positive fluctuation test indicates that the swelling might contains fluid
l) Fluid thrill
Only swelling which contains fluid transmits percussion waves.
Use one of the finger to tap one end of the lump, and feel for the vibration produced at another end, using another finger from another hand.
If the swelling is too large, the percussion wave might be transmitted through the wall.
Hence, one should place a hand at the middle of the swelling to prevent such transmission.
m) Transillumination
If the swelling contains clear fluid, it transilluminate.
It should be done using a small bright light source, in a dark room.
Eg, hydrocele, epididymal cyst
n) Pulsatility
Place one finger of each hand over two ends of the swelling.
If both the fingers are moving upwards and outwards -> expansile (eg, aneurysm)
If both the fingers are moving only upwards (one direction) -> transmitted (a lump overlying an artery)
o) Compressibility
As pressure is applied to the swelling, it's compressed.
But once the pressuring hand is removed, the swelling immediately reappears.
p) Bruits
q) Reducibility
This is different from compressibility.
If the swelling is reducible, it is reduced into another space.
As the pressuring hand is removed, the swelling usually takes some time before reappearing, or will only reappear when there's stimulus, eg cough
r) Relation with surrounding tissue
Is it pinchable from the skin?
When the muscle is tensed,
Does it becomes more prominent, less mobile or less prominent and less easily felt?
When the swelling overlies a nerve/or artery -> not mobile along it's course, but mobile across it's length
s) Any palpable regional lymph nodes?
t) General examination
1. When do you first notice the lump?
REMEMBER, first noticed the lump 3 months ago is not the same as first appeared 3 months ago.
2. How do you notice it?
Below are the 3 commonest answers :
a) It's painful
b) I noticed it accidentally
c) Others told me about it
Generally, if the lump is painful, the commonest aetiology is inflammation.
Most of the patients thought that only painful lumps are cancerous.
3. How does the lump disturbs you?
Basically, the question is asking about the associated symptoms.
It can be pain, discharge, dysphagia, dyspnoea, cosmetically disfiguring, fear of malignancy, etc.
4. Any changes to the lump since you first notice it?
The commonest change is the size.
Whether the lump has increased or decreased in size, or it's size fluctuates.
5. Has the lump ever dissapears before?
Does the lump dissapears when the patient is lying down supine?
or any other activities
6. Do you ever had any other lumps before this?
Asking for multiplicity
7. What do you think is the cause?
Particularly important if there's history of trauma
On examination :
Note the -
a) Position
b) Colour and texture of skin over swelling
c) Size
d) Shape
e) Surface
f) Temperature
g) Tenderness
h) Edge - indistinct/well-defined
i) Composition
Calcified tissues/bone makes the swelling hard
Swelling packed with cells : Firm
Or it might contain fluid (lymph, blood, pus)
Intravascular blood
Gas
j) Consistency
Stony hard - not indentable at all, as hard as bone
Firm - hard, but not as hard as bone
Rubbery - slightly indentable, feels like rubber
Spongy - indentable, but with some resillence
Soft - Squashable, no resillence
k) Fluctuation
Palpate the swelling over 3 planes.
Pressure over the 3rd plane of the swelling usually causes the other 2 planes to buldge out or tensed-up
Positive fluctuation test indicates that the swelling might contains fluid
l) Fluid thrill
Only swelling which contains fluid transmits percussion waves.
Use one of the finger to tap one end of the lump, and feel for the vibration produced at another end, using another finger from another hand.
If the swelling is too large, the percussion wave might be transmitted through the wall.
Hence, one should place a hand at the middle of the swelling to prevent such transmission.
m) Transillumination
If the swelling contains clear fluid, it transilluminate.
It should be done using a small bright light source, in a dark room.
Eg, hydrocele, epididymal cyst
n) Pulsatility
Place one finger of each hand over two ends of the swelling.
If both the fingers are moving upwards and outwards -> expansile (eg, aneurysm)
If both the fingers are moving only upwards (one direction) -> transmitted (a lump overlying an artery)
o) Compressibility
As pressure is applied to the swelling, it's compressed.
But once the pressuring hand is removed, the swelling immediately reappears.
p) Bruits
q) Reducibility
This is different from compressibility.
If the swelling is reducible, it is reduced into another space.
As the pressuring hand is removed, the swelling usually takes some time before reappearing, or will only reappear when there's stimulus, eg cough
r) Relation with surrounding tissue
Is it pinchable from the skin?
When the muscle is tensed,
Does it becomes more prominent, less mobile or less prominent and less easily felt?
When the swelling overlies a nerve/or artery -> not mobile along it's course, but mobile across it's length
s) Any palpable regional lymph nodes?
t) General examination
Urology - Q & A
What are the common causes of urinary tract obstruction?
Upper UT obstruction :
Renal, ureteric calculi
Pelvi-ureteric junction obstruction
Retroperitoneal fibrosis (idiopathic, malignancy)
Transitional cell carcinoma
Congenital (Ectopic ureter, ureterocele)
Infections (Schistosomiasis, TB)
Lower UT obstruction :
Urethral causes (stricture, tumour, stone)
Prostate (BPH, CA prostate)
Bladder neck (CA, stones, neurological causes, stricture)
What are the clinical features of acute urinary retention?
Patient usually complains of suprapubic pain, unable to pass urine
Well aware that there's bladder distension
On examination, bladder is palpable with the following features :
An ovoid mass originating from the pelvis
Can't get below the swelling
Tense, tender, smooth surface
Gentle pressure increases desire to micturate
Immobile
Percussion - dull
Positive fluid thrill
Sometimes, the bladder can be extending up to the umbilicus
(in cases of acute on chronic urinary retention)
What are the clinical features of chronic urinary retention?
Bear in mind that there're 2 types of chronic UR :
a) High pressure type
Associated with chronic bladder outflow obstruction
Can progress to hydroureter and hydronephrosis and eventually, obstructive renal failure
b) Low pressure type
Associated with bladder atony
Doesn't progress towards renal failure
Symptom-wise, patient is usually unaware that there's bladder distension
Usually, such condition is painless
However, there's both obstructive and irritative symptoms of micturition (as in BPH)
And, there's overflow incontinence :
The patient can pass an apparently normal volume of urine
However, whenever there's raised intra-abdominal pressure, there's dribbling of urine
On examination :
Bladder is usually palpable, upto the umbilicus
Non-tender, not tense
Gentle pressure may not be associated with any increased desire in micturition
Dull note on percussion, +ve fluid thrill
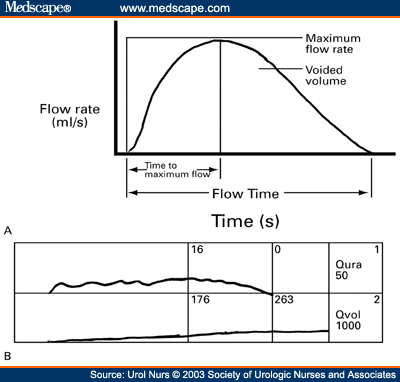
Briefly discuss about the clinical significance of urodynamic studies
Upper UT obstruction :
Renal, ureteric calculi
Pelvi-ureteric junction obstruction
Retroperitoneal fibrosis (idiopathic, malignancy)
Transitional cell carcinoma
Congenital (Ectopic ureter, ureterocele)
Infections (Schistosomiasis, TB)
Lower UT obstruction :
Urethral causes (stricture, tumour, stone)
Prostate (BPH, CA prostate)
Bladder neck (CA, stones, neurological causes, stricture)
What are the clinical features of acute urinary retention?
Patient usually complains of suprapubic pain, unable to pass urine
Well aware that there's bladder distension
On examination, bladder is palpable with the following features :
An ovoid mass originating from the pelvis
Can't get below the swelling
Tense, tender, smooth surface
Gentle pressure increases desire to micturate
Immobile
Percussion - dull
Positive fluid thrill
Sometimes, the bladder can be extending up to the umbilicus
(in cases of acute on chronic urinary retention)
What are the clinical features of chronic urinary retention?
Bear in mind that there're 2 types of chronic UR :
a) High pressure type
Associated with chronic bladder outflow obstruction
Can progress to hydroureter and hydronephrosis and eventually, obstructive renal failure
b) Low pressure type
Associated with bladder atony
Doesn't progress towards renal failure
Symptom-wise, patient is usually unaware that there's bladder distension
Usually, such condition is painless
However, there's both obstructive and irritative symptoms of micturition (as in BPH)
And, there's overflow incontinence :
The patient can pass an apparently normal volume of urine
However, whenever there's raised intra-abdominal pressure, there's dribbling of urine
On examination :
Bladder is usually palpable, upto the umbilicus
Non-tender, not tense
Gentle pressure may not be associated with any increased desire in micturition
Dull note on percussion, +ve fluid thrill
Briefly discuss about the clinical significance of urodynamic studies
The maximum urinary flow rate can be determined by urodynamic studies.
In men, it's 15-30 ml/sec; in females, it's 20-40 ml/sec.
A graph of urinary flow rate versus time can be plotted, in which different pattern of curves usually indicates different causes of obstruction.
A normal urinary flow : Rises to the peak rapidly, and rapidly drops down to the baseline (as shown above)
In bladder outflow obstruction, there's prolonged rise to poor maximum flow rate and periods of prolonged variability in flow rate
In urethral obstruction, there's a stable, plateu-shaped curve, with prolonged flow rate.
Together with cystometry, the bladder capacity, capacity during desire to micturate, pressure on the detrusor muscle in full bladder, residual urine volume can be determined.
History taking in a case of hematuria
First of all, the causes of hematuria :
1) Kidney
Glomerular diseases
Polycystic kidney disease
Kidney stones
Trauma (renal biopsy)
Renal adenocarcinoma
Renal TB
Renal vein thrombosis
Embolism
2) Ureter
Ureteric stones
Neoplasm
3) Bladder
Bladder stones
CA bladder
Bladder Trauma
Inflammation (Cystitis, stones, TB)
4) Prostate
Benign Prostatic Hyperplasia
CA prostate
5) Urethra
Urethral trauma
Urethral stones
Neoplasm
Trauma
General causes
Anticoagulants (Warfarin)
Thrombocytopoenia
Sickle cell disease
Malaria
Schistosomiasis
Blood dyscarias (Hemophilia)
Sternous exercises
Red urine
Hemoglobinuria
Myoglobinuria
Beetroot
Senna
Rifampicin
Phenopthalein
History : Important questions!
1) Is there any pain on micturition?
2) Is it :
Painless hematuria? (Renal TB, RCC, CA bladder)
Total hematuria? (suggestive of bleeding from upper urinary tract)
Initial hematuria? (bleeding from lower urinary tract = prostate?urethra?)
Terminal hematuria? (bleeding from prostate?bladder?)
3) Is there family history of renal disease? (Polycystic)
4) Is there any h/o of drug intake? (anticoagulant)
5) Is there any h/o of substance ingestion that might cause red discolouration of urine?
6) Is there travel history? (Malaria/Schistosomiasis)
7) Is there any fixed loin pain? (Renal causes)
8) Is there any colicky loin to groin pain? (Ureteric colic)
9) Any symptoms suggestive of bladder stones? (Frequency, suprapubic pain, etc)
10) Any symptoms of prostatism?
11) Any h/o of trauma? (including renal biopsy)
12) Any h/o of general debility? (malaise, lost of weight, appetite, etc)
13) Any h/o of bleeding disorders?
14) Any h/o of TB in other parts of body? (esp. pulmonary)
15) Any h/o of sternous exercises done recently?
16) Any h/o of dehydration?
Investigations
1) Full blood count
2) ESR
3) Urine microscopy
4) Chest X-ray
5) Coagulation profile (PT and INR)
6) KUB film or IVU (calculus)
1) Kidney
Glomerular diseases
Polycystic kidney disease
Kidney stones
Trauma (renal biopsy)
Renal adenocarcinoma
Renal TB
Renal vein thrombosis
Embolism
2) Ureter
Ureteric stones
Neoplasm
3) Bladder
Bladder stones
CA bladder
Bladder Trauma
Inflammation (Cystitis, stones, TB)
4) Prostate
Benign Prostatic Hyperplasia
CA prostate
5) Urethra
Urethral trauma
Urethral stones
Neoplasm
Trauma
General causes
Anticoagulants (Warfarin)
Thrombocytopoenia
Sickle cell disease
Malaria
Schistosomiasis
Blood dyscarias (Hemophilia)
Sternous exercises
Red urine
Hemoglobinuria
Myoglobinuria
Beetroot
Senna
Rifampicin
Phenopthalein
History : Important questions!
1) Is there any pain on micturition?
2) Is it :
Painless hematuria? (Renal TB, RCC, CA bladder)
Total hematuria? (suggestive of bleeding from upper urinary tract)
Initial hematuria? (bleeding from lower urinary tract = prostate?urethra?)
Terminal hematuria? (bleeding from prostate?bladder?)
3) Is there family history of renal disease? (Polycystic)
4) Is there any h/o of drug intake? (anticoagulant)
5) Is there any h/o of substance ingestion that might cause red discolouration of urine?
6) Is there travel history? (Malaria/Schistosomiasis)
7) Is there any fixed loin pain? (Renal causes)
8) Is there any colicky loin to groin pain? (Ureteric colic)
9) Any symptoms suggestive of bladder stones? (Frequency, suprapubic pain, etc)
10) Any symptoms of prostatism?
11) Any h/o of trauma? (including renal biopsy)
12) Any h/o of general debility? (malaise, lost of weight, appetite, etc)
13) Any h/o of bleeding disorders?
14) Any h/o of TB in other parts of body? (esp. pulmonary)
15) Any h/o of sternous exercises done recently?
16) Any h/o of dehydration?
Investigations
1) Full blood count
2) ESR
3) Urine microscopy
4) Chest X-ray
5) Coagulation profile (PT and INR)
6) KUB film or IVU (calculus)
Bladder carcinoma
Pathology
Almost all cases of Bladder carcinomas are originating from the transitional epithelium.
Since, the urothelium is frequently exposed to carcinogens that might be excreted through the urine. Urothelium over the bladder is commonly involved since there's always residual urine.
Occasionally, bladder carcinoma might be squamous cell in nature.
This is usually seen when there's chronic inflammation of the bladder mucosa, caused by stones or schistosomiasis.
Rarely, it presents as adenocarcinoma.
Usually due to local infiltration of tumour from pelvic organs, or bowel.
History and examination
Males are 3 times more likely to have CA bladder than females.
Age of presentation is usually around 60-70s.
Certain occupations are at high risk of developing this malignancy, especially those frequently deals with chemical dyes (Naphthylamine and Benzidine):
Leather workers
Painters or decorators
Paper or rubber manufactures
Dental technicians
Painless and terminal or total hematuria present in about 80% of the cases
Sometimes, patients might be passing out blood clots
Hence, there might be dysuria, or difficulty in micturition
If the residual urine gets infected, there's symptoms of cystitis
If the tumours originating from the ureteric orifice of bladder, loin pain can present
If infiltration had taken place to adjacent structures, lower abdominal pain radiating to the legs might be present
Bear in mind that for patients with recurrent cystitis not responding to treatment, think of CA bladder.
On examination, usually is not very helpful.
Mass may be palpable over the suprapubic area, over even during per rectal examination.
TMN staging of bladder carcinoma
Tis - Carcinoma in situ, means tumour cells are present only over the inner lining
Ta - Non-invasive, papillary tumour
T1 - Invasive, however, yet to involve the bladder musculature
T2a and T2b - Infiltration beyond bladder musculature
T3a and T3b - Infiltration into the fatty tissue around the bladder
T4a and T4b - Invasion into the adjacent organs (prostate, pelvic wall)
Investigation
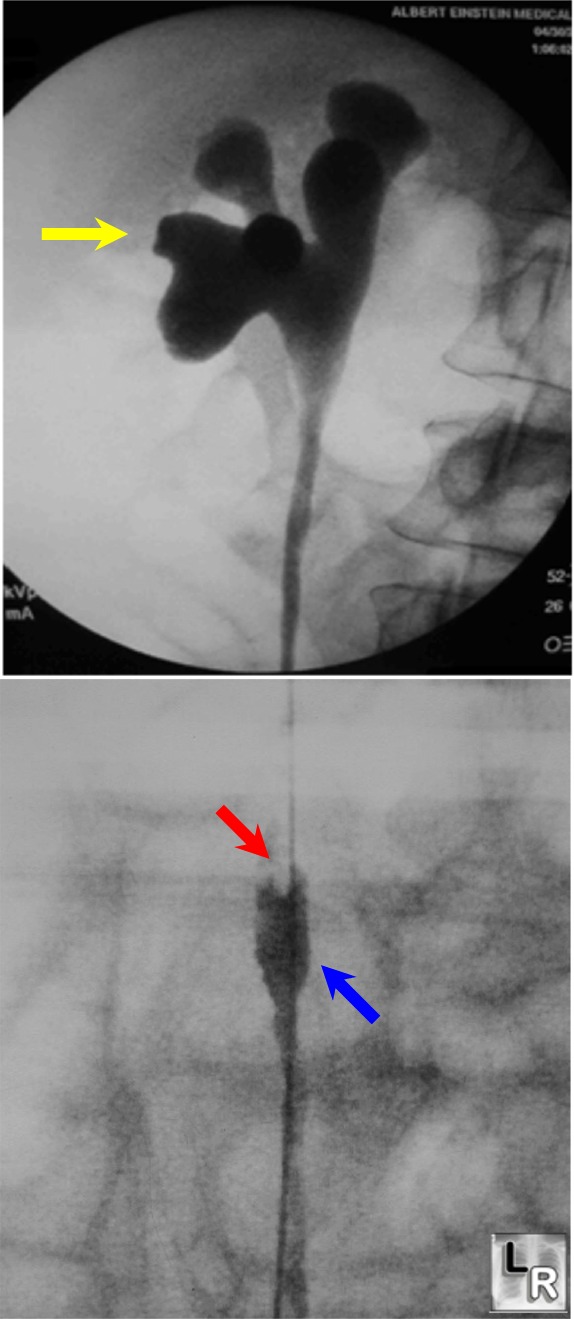
Intravenous urogram will shows filling defect within bladder :
IF such picture is seen, a retrograde ureteropyelogram is indicated
Then, cystourethrography should be done under general anasthesia for examination of the tumour, and biopsy specimen can be taken.
CT abdomen for staging.
Prostatic diseases
The two main disease of the prostate :
1) Benign prostatic hyperplasia (BPH)
In brief, what happens is as men ages (>45 yrs), testosterone levels are reduced and the levels can be relatively lower than the estrogen levels.
Hence, estrogenic effects over the prostate causes proliferation, first over the periurethral region.
1) Benign prostatic hyperplasia (BPH)
In brief, what happens is as men ages (>45 yrs), testosterone levels are reduced and the levels can be relatively lower than the estrogen levels.
Hence, estrogenic effects over the prostate causes proliferation, first over the periurethral region.
Note that as the prostate enlarges, it compresses on and elongates the prostatic urethra. Hence, it results in symptoms of bladder outflow obstruction.
Initially, higher pressure is required to force the urine out of the bladder and as it becomes chronic, bladder muscular hypertrophy occurs.
Trabeculum formation occurs and as it saccules, bladder diverticulum forms.
These bladder diverticulum can result in 3 complications of urinary stasis :
Infection, Stones and Tumour
Eventually, these bladder diverticulum causes increased residual urinary volume and hence, back-pressure to the ureter and kidney occurs and hence resulting in hydroureter or even hydronephrosis.
What are the clinical features?
Symptoms usually becomes clinically apparent beyond 50 yrs of age.
1) Frequency
Patient noticed that there's increased frequency of micturition.
This is especially noticable when there's nocturia.
2) Urgency
Patient complains that he can no longer hold his desire to urinate.
There's an urgent need to pass urine once there's desire to urinate.
Sometimes can be associated with incontinence.
3) Hesitancy
Although there's intense desire to micturate, but the waiting time for the urine to start flowing out is delayed.
In other words, there's difficulty in initiating micturation.
4) Poor stream
Yes, there's a weak urinary stream.
5) Terminal dribbling
After cessation of the main stream, usually it ends with terminal dribbling.
As the patient loses his patience, the urine stains the underclothing.
6) Hematuria
Usually an initial or terminal hematuria
7) Uremia
Sometimes, patients can present with features of uremia.
On examination
Look for features of uraemia.
Bladder may be palpable when there's urinary retention.
Per rectal examination :
Remember to ask the patient to pass urine before examining the prostate.
The prostate is diffusely, however asymmetrically enlarged.
Surface, although smooth, can be bosselated since the enlargement is non-uniformed.
The consistency is usually rubbery, firm and homogenous.
Median sulcus of prostate is palpable, and the rectal mucosa overlying the gland is freely mobile.
2) CA prostate
Most common malignancy among men.
Age of presentation is usually around 80s-90s.
Basically, the symptoms are indistinguishable from BPH.
However, in addition to prostatism, other symptoms suggestive of CA prostate includes :
General debility (weight loss, malaise, body weakness, anorexia)
Bony pain (note that the metastatic deposits are osteosclerotic in nature, hence pathological fractures are actually uncommon)
As the tumour invades the adjacent structures, it may cause severe lower abdominal or perineal pain.
On examination -
Bony tenderness
PR examination reveals an asymmetrically enlarged gland, which is distorted and with a irregular, craggy surface.
The consistency is variable/knobbly, as some areas may be stony hard, others may be soft.
The median sulcus may not be palpable, and the rectal mucosa overlying the gland may be fixed.
Investigations
Any patient presents with BPH should be opted for CA prostate screening as well.
a) Full blood count and BUSE
FBC - to look for renal anemia
BUSE - evaluate renal function
b) Serum PSA
Serum PSA of >100ng/ml is significant for distant metastases.
c) Midstream urine collected for urine culture
To rule out urinary tract infections
d) Chest X-ray/X-ray of the spine
For any evidence of metastases
e) Urodynamic studies
f) If malignancy is suspected, prepare a transrectal ultrasonographic guided needle biopsy of the prostate.
Management
For BPH,
1) Symptommatic
If renal function is normal, and CA prostate has been ruled out, initial management should be medical.
For short-term relief of symptoms, start alpha-blockers (terazosin, tamsulosin)
Start finasteride therapy, which inhibits conversion of testosterone to dihydrotestosterone. Hence, this reduces the size of prostate gland.
It will require few months before this drugs start to exhibit it's effect.
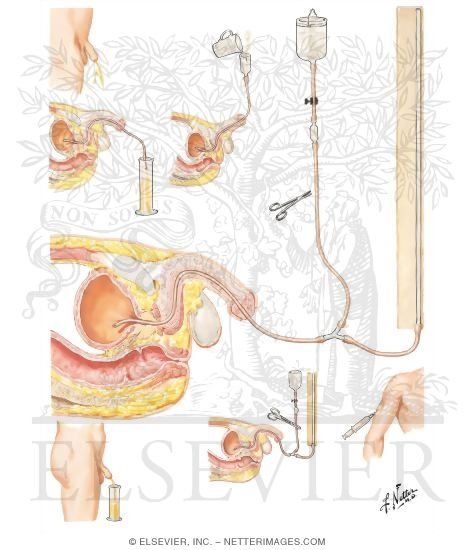
2) Acute retention
If patient presents with acute urinary retention :
a) Admit the patient
b) Urinary catheterisation with strict asepsis
c) If not possible, start suprapubic aspiration using a wide cannula
d) Urinary catheter can be kept for 24-48 hrs at most. However, if the urinary symptoms are less, urinary catheter can be removed after 12 hrs. (Prescrbie alfuzosin 10mg/day after that)
3) Chronic retention
First, rule out malignancy and renal function impairment.
If there's renal function impairment leading to electrolyte imbalance (hyperkalemia, hypocalcemia, hyperphosphatemia), correct it first.
Then, only plan for prostectomy
For CA prostate,
1) For indicental focal findings of malignancy :
If the cells are well-differentiated -> wait-and-see
If cells are undifferentiated -> surgery + radiotherapy*
2) Localised malignancy without bony metastases :
Surgery + radiotherapy*
* : only for those with life-expectancy >10yrs
3) With bony metastases
Orchidectomy or start GnRH analogues
Urinary stones
Introduction
Hence, there's a stabbing lower abdominal pain or intense desire to micturate.
While lying down supine, symptoms subsided since the stones fall away from the trigone.
There might be intermittent cessation of urinary flow due to the same reason.
Other symptoms includes : hematuria, features of cystitis (suprapubic pain, burning micturition)
Investigations
A pain abdominal X-ray may reveal a radio-opaque lesion seen along the course of ureter.
Usually, an intravenous urogram reveals obstruction caused by the stones.
Midstream urine is sent for urine culture to rule out any infection.
Renal profile is evaluated
Management
First of all, IM diclofenac is to be given to relief pain (pethidine is an alternative)
In case where the stones are <0.5cm in diameter, as it passes out spontaneously, and the patient's condition improves, there's no further interventions required.
However, if there's evidence of hydroureter, hydronephrosis, increasing pain/fever, treatment is required.
Management of choice nowadays is the extracorporal shock wave lithotripsy.
Alternatively, a ureteroscope is inserted to break the stones.
Or in case where the above 2 interventions fails, go for percutaneous nephrolithotomy.
Urinary stones are usually divided into 2 types :
1) Infective
These stones are usually whitish and chalky, and they crumbles easily.
Usually due to impaired drainage of urine, for eg, in cases of prolonged immobilisation or even bladder diverticulum.
Main constituents includes calcium, ammonia, and magnesium phosphate.
2) Metabolic
80% of these stones are calcium-oxalate stones.
Usually due to abnormal concentration of normal constituents (dehydration) Or
presence of abnormal constituents in urine (homocystinuria) Or
excessive amount of normal constituents in urine (hypercalcemia secondary to hyperparathyroidism or hyperuricemia due to gout)
Hence, any recurrent renal/ureteric colic is an indication for such metabolic screening.
Renal and ureteric stones
More common in males, aged in between 30-50 years of age.
The predominant symptom here is pain, which is dependent on the site of the stones.
If it's a renal stone, it causes a dull, sometimes severe fixed renal pain at the loin (region in between the 12th rib and iliac crest)
Once it has entered into the ureter, the pain changes it's nature.
It becomes colicky (in fact, a true colic), radiating from the loin to groin, testes, labia, and even to the tip of penis.
And of course, the pain might be the worst pain ever experience by the patient.
The patient will be jolting around, rolling, in attempt to relieve the pain.
And it's associated with nausea and vomiting.
Macroscopic hematuria is usually not seen.(although evidence of microscopic hematuria more common)
Bear in mind that the first presentation might be in the form of acute pyelonephritis (triad = fever, loin pain, dysuria)
Or some stones can be clinically silent, till it produces significant renal impairment where the patient first presents with features of uraemia.
It's not possible to examine the patient while he/she is having acute pain. Hence, diagnosis is mostly from history.
Bladder stones
Bladder stones are more commonly seen in middle-age and elderly patients.
Most of them are having prostatic diseases.
Common symptoms include increased frequency of micturition, which sometimes can be related to posture.
While standing up, the stones fall onto the bladder trigone.Hence, there's a stabbing lower abdominal pain or intense desire to micturate.
While lying down supine, symptoms subsided since the stones fall away from the trigone.
There might be intermittent cessation of urinary flow due to the same reason.
Other symptoms includes : hematuria, features of cystitis (suprapubic pain, burning micturition)
Investigations
A pain abdominal X-ray may reveal a radio-opaque lesion seen along the course of ureter.
Usually, an intravenous urogram reveals obstruction caused by the stones.
Midstream urine is sent for urine culture to rule out any infection.
Renal profile is evaluated
Management
First of all, IM diclofenac is to be given to relief pain (pethidine is an alternative)
In case where the stones are <0.5cm in diameter, as it passes out spontaneously, and the patient's condition improves, there's no further interventions required.
However, if there's evidence of hydroureter, hydronephrosis, increasing pain/fever, treatment is required.
Management of choice nowadays is the extracorporal shock wave lithotripsy.
Alternatively, a ureteroscope is inserted to break the stones.
Or in case where the above 2 interventions fails, go for percutaneous nephrolithotomy.
Renal adenocarcinoma
Introduction
It's the commonest malignant tumour of the kidney, also known as hypernephroma.
The peak incidence is around the age of 50-70s, male predominance.
The tumour arises from the renal tubules.
Early spread is common in Renal adenocarcinoma :
a) Direct - involving the perinephric tissue, extension into the renal veins, and then the IVC
b) Lymphatic - involving the ipsilateral para-aortic lymph nodes
c) Hematogenous - pelvic bone, vertebras, lungs, etc
Clinical features
1) History suggestive of RCC
Painless hematuria (usually a total hematuria)
General debility (lost of weight, appetite, malaise, weakness)
Bony pain and pathological fractures
Fixed loin pain (pressure over the renal capsule)
Occasionally, a loin mass is felt by the patient
Less common presentations :
a) Pyrexia of unknown origin
b) Varicocele/Bilateral pedal edema
Extension of the tumour involving the left gonadal veins or into the IVC
c) Polycythemia
Excessive production of erythropoeitin from the malignant cells
Facial, skin over palm/soles redness, recurrent venous/arterial thromboses
d) Sudden severe abdominal pain
Haemorrhage into the tumour
e) Hypertension - rare complication
2) On examination
Evidence of recent weight lost
Palpable loin mass, kidney (ballotable), may be tender
Bony tenderness
Evidence of lung metastases
Investigations
Renal ultrasound
CT abdomen, mainly for staging
Treatment
RCC is a radio and chemoresistant tumour, hence the only option is radical nephrectomy, including the perinephric tissue and ipsilateral para-aortic lymph nodes.
It's the commonest malignant tumour of the kidney, also known as hypernephroma.
The peak incidence is around the age of 50-70s, male predominance.
The tumour arises from the renal tubules.
Early spread is common in Renal adenocarcinoma :
a) Direct - involving the perinephric tissue, extension into the renal veins, and then the IVC
b) Lymphatic - involving the ipsilateral para-aortic lymph nodes
c) Hematogenous - pelvic bone, vertebras, lungs, etc
Clinical features
1) History suggestive of RCC
Painless hematuria (usually a total hematuria)
General debility (lost of weight, appetite, malaise, weakness)
Bony pain and pathological fractures
Fixed loin pain (pressure over the renal capsule)
Occasionally, a loin mass is felt by the patient
Less common presentations :
a) Pyrexia of unknown origin
b) Varicocele/Bilateral pedal edema
Extension of the tumour involving the left gonadal veins or into the IVC
c) Polycythemia
Excessive production of erythropoeitin from the malignant cells
Facial, skin over palm/soles redness, recurrent venous/arterial thromboses
d) Sudden severe abdominal pain
Haemorrhage into the tumour
e) Hypertension - rare complication
2) On examination
Evidence of recent weight lost
Palpable loin mass, kidney (ballotable), may be tender
Bony tenderness
Evidence of lung metastases
Investigations
Renal ultrasound
CT abdomen, mainly for staging
Treatment
RCC is a radio and chemoresistant tumour, hence the only option is radical nephrectomy, including the perinephric tissue and ipsilateral para-aortic lymph nodes.
Anatomy of the Urinary system
Upper urinary tract
Both kidneys are situated retroperitoneally on the posterior abdominal wall.
The left kidney is higher than the right kidney.
The diagphram separates the superior poles of both kidneys from the pleura, the 11th and 12th ribs.
Both kidneys are overlying the psoas major, quadratus lumborum, and transversus abdominis from medial to lateral side.
Anteriorly, the right kidney is overlied by the 2nd part of duodenum, ascending colon, and the liver; whilst the left kidney is overlied by the spleen, stomach, tail of pancreas, and the descending colon.
At the hilum, the front-most structure is the renal veins, followed by renal artery and lastly the renal pelvis.
Both kidneys are situated retroperitoneally on the posterior abdominal wall.
The left kidney is higher than the right kidney.
The diagphram separates the superior poles of both kidneys from the pleura, the 11th and 12th ribs.
Both kidneys are overlying the psoas major, quadratus lumborum, and transversus abdominis from medial to lateral side.
Anteriorly, the right kidney is overlied by the 2nd part of duodenum, ascending colon, and the liver; whilst the left kidney is overlied by the spleen, stomach, tail of pancreas, and the descending colon.
At the hilum, the front-most structure is the renal veins, followed by renal artery and lastly the renal pelvis.
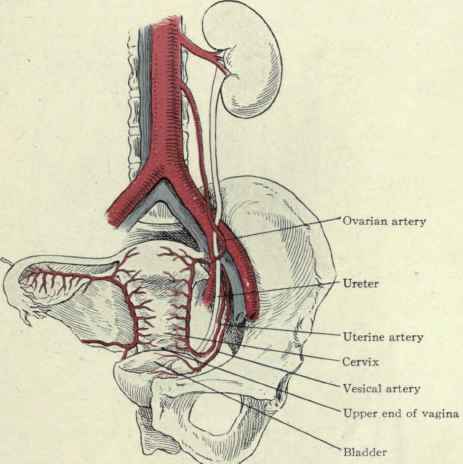
The abdominal ureters runs over the medial edge of the psoas major muscles, which separates it from the transverse process of the vertebras.
Then, it crosses over the bifurcation of the common iliac artery, which separates it from the sacroiliac joint.
Once it gain entry into the pelvis, it runs over the lateral pelvic wall, passing through the ischial spine.
Finally, it runs medially and enters the bladder.
Note the 3 most common site of stone impaction : Pelvi-ureteric junction, Pelvic brim, and the ureteric orifice.
Lower urinary tract
Upto 4 years of age, the bladder is an abdominal organ.
In adults, the bladder is a pelvic organ, well protected by the pelvic bone.
Superiorly, it is separated from the sigmoid colon, and loops of small bowel by a fold of peritoneum. (in females, the body of uterus as well)
Posteriorly, it's related to the seminal vesicles and vas deferens, and the rectum, in the case of male.
Whereas in females, it's related to the supravaginal cervix and vagina.
In males, the neck of bladder is encircled by the prostate, whereas in females, it fuses with the pelvic fascia.
The length of urethra is males is about 20cm, whilst in females, 3-4cm.
In male urethra, it's divided into prostatic urethra, bulbar urethra and penile urethra. The penile urethra is covered by corpus spongiosum.
It opens out to the tip of glans penis lastly.
Friday, November 20, 2009
Colon Cancer - Q & A
What are the risk factors?
Age > 45 yrs
Lack of dietary fibers & High protein diet (meat)
Alcoholism, Smoking
Cholecystectomy - increased bile acid secretion
Explain briefly the pathology.
Histologically - columnar cell neoplasm
Macroscopically, it's divided into 4 types : annular, tubular, ulcerative and cauliflower type.
Annular type causes predominantly obstructive symptoms, whilst others causes bleeding more often.
Enumerate some common sites involved.
Rectum (most common)
Sigmoid colon
Descending colon
Caecum
Explain the clinical features.
a) Carcinoma of caecum + ascending colon
Patient presents mostly with features of anaemia, weight lost or sometimes abdominal mass. Abdominal pain is not a usual symptoms, however if present, usually is dull aching, or colicky in nature, over the right lower quadrant.
On examination, the patient is usually pale and appears wasted.
If the patient is thin enough, a mass may be visible over the RIF or the right lumbar region, confirmed by palpation, which is usually hard, mobile/fixed.
Percussion over the mass - dull note.
Normal bowel sounds are usually heard.
It's possible that CA caecum can triggers episode of acute appendicitis in such patients. More importantly, there's no difference in the clinical features from the usual ones. Hence, any patient, >45 yrs of age, presented with acute appendicitis, CA caecum should also be suspected. The other differential diagnosis includes :
Caecal diverticulum
Ileocaecal tuberculosis
Crohn's disease
b) Carcinoma involving the left sided colon
The age of the patient is usually >45yrs old.
However, if it involves younger patients (20-30), suspect familial polyposis/or it can even occurs as a complication of long-standing ulcerative colitis.
There's no sexual predilection.
The first complaint is usually altered bowel habits.
There's usually a period of constipation, interpersed in between periods of explosive diarrhoea.
The constipation is obviously caused by obstruction, and diarrhoea is caused by liquefaction of the stools above the obstruction.
Sometimes, the diarrhoea can be worsened by passing mucuos, as when the surrounding colonic mucosa gets inflammed.
Per rectal bleeding is also an important symptom.
The blood is usually dark-plum coloured, sometimes accompanied by some amount of clots.
Especially when the tumour involves sites such as the rectosigmoid junction, it can easily prolapsed into the rectum, causing tenesmus.
Tenesmus is defined as intense desire to evacuate the bowel, but however, nothing passes out (or scanty amount of loose stools) when the patient tried to pass motion.
Commonly associated with sensation of incomplete bowel evacuation.
Lastly, pain is again not a usual feature.
Some amount of dull-aching, or colicky pain may be appreciated over the left lower quadrant of abdomen.
Weight lost usually occurs before anorexia develops.
On examination, patient is wasted.
Mass may be visible/felt over the left iliac fossa or the left lumbar region.
In can be tender when associated with areas of inflammation around the mass.
Indentation of the abdomen at proximal sites may be possible - stool collection
Dull note on percussion over the mass.
Normal bowel sounds are usually heard.
However, if the patient neglects the above symptoms, it can complicates as bowel perforation, that surprisingly, occurs at the caecum instead of the site of malignancy.
Patient can presents with severe generalised abdominal pain, with features of shock.
What are the mode of spreading for CA colon?
1) Direct spread
Longituidinal, transverse or radial.
It usually involves the surrounding bowel wall causing obstruction before invading the adjacent structures.
Sometimes, fistulas are formed when the tumour invades to adjacent structures (vesico-enteric fistula)
Radial spread involving the adjacent organ determines the prognosis.
2) Lymphatic spread
Lymph nodes draining the colon :
L1 -> Nodes located within the vicinity of the colon
L2 -> Right, left colic, mid-colic and ileocolic nodes
L3 -> Nodes originating from the abdominal aorta, close to the superior mesenteric vessels
3) Hematogenous spread
Via the portal system, it spreads to the liver.
Rarely to the skin, lungs, brain
4) Transcoelomic spread
What are the investigations to be done?
Currently, colonscopy is the investigation of choice, provided that the patient is fit enough to undergo bowel preparation.
The advantage is, not only the primary tumour can be clealy visible, but any polyps or other synchronous tumour.
However, it carries a small risk of bowel perforation.
If colonoscopy is contraindicated, Double contrast barium studies can be done.
On abdominal X-ray, we'll be looking for a filling-defect.
Or flexible sigmoidoscopy can be done.
Ultrasound of the liver to look for secondaries.
CT abdomen, thorax as for staging of the malignancy.
Age > 45 yrs
Lack of dietary fibers & High protein diet (meat)
Alcoholism, Smoking
Cholecystectomy - increased bile acid secretion
Explain briefly the pathology.
Histologically - columnar cell neoplasm
Macroscopically, it's divided into 4 types : annular, tubular, ulcerative and cauliflower type.
Annular type causes predominantly obstructive symptoms, whilst others causes bleeding more often.
Enumerate some common sites involved.
Rectum (most common)
Sigmoid colon
Descending colon
Caecum
Explain the clinical features.
a) Carcinoma of caecum + ascending colon
Patient presents mostly with features of anaemia, weight lost or sometimes abdominal mass. Abdominal pain is not a usual symptoms, however if present, usually is dull aching, or colicky in nature, over the right lower quadrant.
On examination, the patient is usually pale and appears wasted.
If the patient is thin enough, a mass may be visible over the RIF or the right lumbar region, confirmed by palpation, which is usually hard, mobile/fixed.
Percussion over the mass - dull note.
Normal bowel sounds are usually heard.
It's possible that CA caecum can triggers episode of acute appendicitis in such patients. More importantly, there's no difference in the clinical features from the usual ones. Hence, any patient, >45 yrs of age, presented with acute appendicitis, CA caecum should also be suspected. The other differential diagnosis includes :
Caecal diverticulum
Ileocaecal tuberculosis
Crohn's disease
b) Carcinoma involving the left sided colon
The age of the patient is usually >45yrs old.
However, if it involves younger patients (20-30), suspect familial polyposis/or it can even occurs as a complication of long-standing ulcerative colitis.
There's no sexual predilection.
The first complaint is usually altered bowel habits.
There's usually a period of constipation, interpersed in between periods of explosive diarrhoea.
The constipation is obviously caused by obstruction, and diarrhoea is caused by liquefaction of the stools above the obstruction.
Sometimes, the diarrhoea can be worsened by passing mucuos, as when the surrounding colonic mucosa gets inflammed.
Per rectal bleeding is also an important symptom.
The blood is usually dark-plum coloured, sometimes accompanied by some amount of clots.
Especially when the tumour involves sites such as the rectosigmoid junction, it can easily prolapsed into the rectum, causing tenesmus.
Tenesmus is defined as intense desire to evacuate the bowel, but however, nothing passes out (or scanty amount of loose stools) when the patient tried to pass motion.
Commonly associated with sensation of incomplete bowel evacuation.
Lastly, pain is again not a usual feature.
Some amount of dull-aching, or colicky pain may be appreciated over the left lower quadrant of abdomen.
Weight lost usually occurs before anorexia develops.
On examination, patient is wasted.
Mass may be visible/felt over the left iliac fossa or the left lumbar region.
In can be tender when associated with areas of inflammation around the mass.
Indentation of the abdomen at proximal sites may be possible - stool collection
Dull note on percussion over the mass.
Normal bowel sounds are usually heard.
However, if the patient neglects the above symptoms, it can complicates as bowel perforation, that surprisingly, occurs at the caecum instead of the site of malignancy.
Patient can presents with severe generalised abdominal pain, with features of shock.
What are the mode of spreading for CA colon?
1) Direct spread
Longituidinal, transverse or radial.
It usually involves the surrounding bowel wall causing obstruction before invading the adjacent structures.
Sometimes, fistulas are formed when the tumour invades to adjacent structures (vesico-enteric fistula)
Radial spread involving the adjacent organ determines the prognosis.
2) Lymphatic spread
Lymph nodes draining the colon :
L1 -> Nodes located within the vicinity of the colon
L2 -> Right, left colic, mid-colic and ileocolic nodes
L3 -> Nodes originating from the abdominal aorta, close to the superior mesenteric vessels
3) Hematogenous spread
Via the portal system, it spreads to the liver.
Rarely to the skin, lungs, brain
4) Transcoelomic spread
What are the investigations to be done?
Currently, colonscopy is the investigation of choice, provided that the patient is fit enough to undergo bowel preparation.
The advantage is, not only the primary tumour can be clealy visible, but any polyps or other synchronous tumour.
However, it carries a small risk of bowel perforation.
If colonoscopy is contraindicated, Double contrast barium studies can be done.
On abdominal X-ray, we'll be looking for a filling-defect.
Or flexible sigmoidoscopy can be done.
Ultrasound of the liver to look for secondaries.
CT abdomen, thorax as for staging of the malignancy.
Thursday, November 19, 2009
Inguinal and Femoral Hernia
Anatomy of Inguinal canal
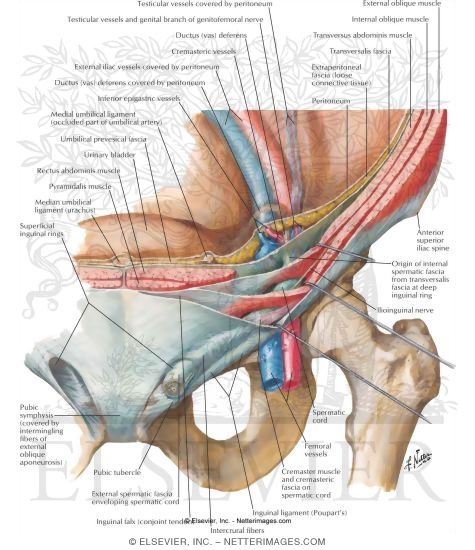
The inguinal canal is about 3.75cm in length, extending from the superficial to deep inguinal ring.
The superficial, or external inguinal ring is an opening of the external oblique aponeurosis, located about 1.25cm above the pubic tubercle. It's lined by superomedial and inferolateral crural fibers.
The deep inguinal ring is a U-shaped condensation of the fascia transversalis, located 1.25cm above the mid-inguinal point (midpoint of a line joining the ASIS to the pubic symphysis)
The boundaries of inguinal canal :
a) Anterior : External oblique aponeurosis and cojoined msucles laterally (1/3)
b) Posterior : Fascia transversalis and conjoined tendon medially (2/3)
c) Floor : Inguinal ligament
d) Roof : Internal oblique and Transversus abdominis muscles (the conjoined muscles)
In males, the spermatic cord, genital branch of genitofemoral nerve, and ilioinguinal nerve traverses through the canal
In females, it's replaced by the round ligament of uterus.
Remember the contents of spermatic cord :
2 nerves : genital branch of genitofemoral nerve + ilioinguinal nerve
2 vessels : cremesteric artery, testicular artery
2 structures : pampiniform venous plexus, lymphatics
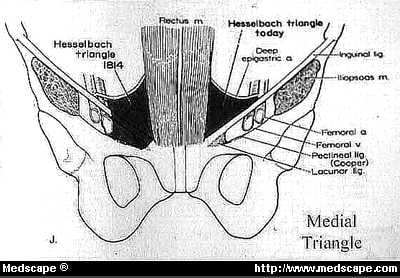
Noticed that the inferior epigastric artery lies medial to the internal inguinal ring. The triangular area bounded medially by the lateral border of rectus abdominis, laterally by inferior epigastric artery and inferiorly by the inguinal ligament is known as the Hesselbach's triangle.
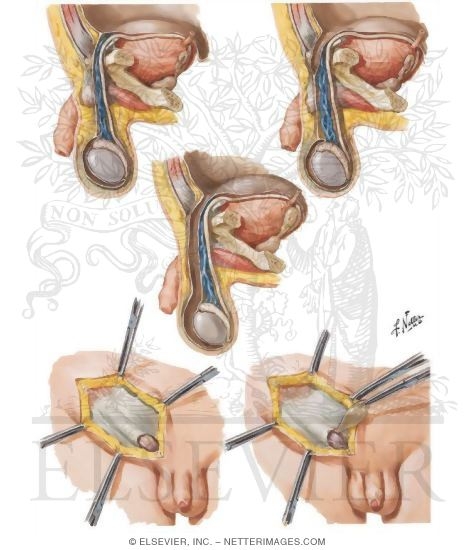
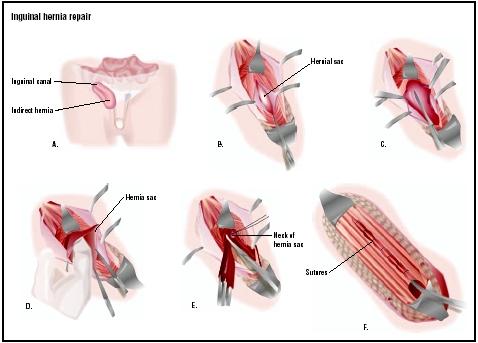
In case of indirect inguinal hernia, the abdominal contents enters through the deep inguinal ring, traverses through the canal, and exits through the superficial inguinal ring.
In case of direct inguinal hernia, it protrudes directly through the Hesselbach's triangle without entering the deep inguinal ring.
Anatomy of the Femoral canal
The femoral canal overlies the medialmost compartment of the femoral sheath, extending from the femoral ring above to the saphenous opening below.
It's about 1.25cm in length and width, and contains cloquet's node, lymphatic vessels and fat.
The above is closed by septum crurale, whilst below is by the cribiform fascia.
The boundaries of femoral ring :
Anterior : Inguinal ligament
Posterior : Pubic bone, Pectineal fascia, iliopectineal ligament
Medial : Lacunar ligament
Lateral : Septum that divides it from the femoral vein
Inguinal hernia
A hernia is defined as an abnormal protrusion of a viscus (or part of it) through an abdominal opening of the wall of it's containing cavity.
Before discussing about inguinal hernia, there's some basic concepts must be understood first.
Composition of hernia :
1) The sac
2) The coverings of sac
3) The contents of sac
Possible contents of the sac :
Omentum -> Omentocele
Intestines -> Enterocele
Ovary without fallopian tubes
Part of the bladder
Circumferential part of an intestine (Ritcher's Hernia)
Meckel's diverticulum (Littre's Henia)
5 clinical types of Hernia :
1) Reducible hernia
It means the hernia can be reduced, either spontaneously when the patient lies down supine, or manually.
For enterocele, the initial part of reduction is difficult. A gurgling sound is usually heard.
For omentocele, the initial part of reduction is easy, but the terminal part is difficult.
2) Irreducible hernia
Usually occurs due to adhesion occurs in between the neck of the sac and contents or even when there's overcrowding of contents.
Other than the irreducibility, there's no other abnormalities.
There's a risk of strangulation at any time.
3) Obstructed hernia
It means the intestinal loop within the hernial sac is obstructed.
Presents with cardinal features of intestinal obstruction.
Eventually progresses towards strangulation.
4) Strangulated hernia
In this case, not only there's bowel obstruction, but with ischaemia of the contents within the sac.
Gangrene of the contents usually occurs 5-6 hours after the onset.
There are 2 types of inguinal hernia :
1) Direct inguinal hernia
It's an accquired hernia.
Almost always seen in elderly, or individuals with the nature of occupation is lifting heavy weights (manual labourers).
Previous apendicectomy, which involves an accidental removal of the ilioinguinal nerve predisposes to direct inguinal hernia, since it weakens the abdominal wall.
The size of hernia is usually small, and rarely descends down to the scrotum.
Since the neck of the hernia is wide, direct inguinal hernia rarely strangulates.
2) Indirect inguinal hernia
Types of indirect inguinal hernia :
1) Bubonocele - The extent of protrusion of the viscus is within the canal
2) Funicular - The processus vaginalis obliterates just above the epididymis. Hence, the hernia is separately palpable from the testis (above it)
3) Complete - extending from the deep inguinal ring, through the canal, exits the superficial ring and down to the scrotum.
Differential diagnosis of inguinal hernia :
a) In males :
1) Vaginal hydrocele
2) Femoral hernia
3) Encysted hydrocele of the cord
4) Lipoma of the cord
5) Undescended testis within the canal
b) In females
1) Femoral hernia
2) Hydrocele of the canal of nuck
Femoral hernia
Note, is it right/left sided or bilateral?
The superficial, or external inguinal ring is an opening of the external oblique aponeurosis, located about 1.25cm above the pubic tubercle. It's lined by superomedial and inferolateral crural fibers.
The deep inguinal ring is a U-shaped condensation of the fascia transversalis, located 1.25cm above the mid-inguinal point (midpoint of a line joining the ASIS to the pubic symphysis)
The boundaries of inguinal canal :
a) Anterior : External oblique aponeurosis and cojoined msucles laterally (1/3)
b) Posterior : Fascia transversalis and conjoined tendon medially (2/3)
c) Floor : Inguinal ligament
d) Roof : Internal oblique and Transversus abdominis muscles (the conjoined muscles)
In males, the spermatic cord, genital branch of genitofemoral nerve, and ilioinguinal nerve traverses through the canal
In females, it's replaced by the round ligament of uterus.
Remember the contents of spermatic cord :
2 nerves : genital branch of genitofemoral nerve + ilioinguinal nerve
2 vessels : cremesteric artery, testicular artery
2 structures : pampiniform venous plexus, lymphatics
Noticed that the inferior epigastric artery lies medial to the internal inguinal ring. The triangular area bounded medially by the lateral border of rectus abdominis, laterally by inferior epigastric artery and inferiorly by the inguinal ligament is known as the Hesselbach's triangle.
In case of indirect inguinal hernia, the abdominal contents enters through the deep inguinal ring, traverses through the canal, and exits through the superficial inguinal ring.
In case of direct inguinal hernia, it protrudes directly through the Hesselbach's triangle without entering the deep inguinal ring.
Anatomy of the Femoral canal
The femoral canal overlies the medialmost compartment of the femoral sheath, extending from the femoral ring above to the saphenous opening below.
It's about 1.25cm in length and width, and contains cloquet's node, lymphatic vessels and fat.
The above is closed by septum crurale, whilst below is by the cribiform fascia.
The boundaries of femoral ring :
Anterior : Inguinal ligament
Posterior : Pubic bone, Pectineal fascia, iliopectineal ligament
Medial : Lacunar ligament
Lateral : Septum that divides it from the femoral vein
Inguinal hernia
A hernia is defined as an abnormal protrusion of a viscus (or part of it) through an abdominal opening of the wall of it's containing cavity.
Before discussing about inguinal hernia, there's some basic concepts must be understood first.
Composition of hernia :
1) The sac
2) The coverings of sac
3) The contents of sac
Possible contents of the sac :
Omentum -> Omentocele
Intestines -> Enterocele
Ovary without fallopian tubes
Part of the bladder
Circumferential part of an intestine (Ritcher's Hernia)
Meckel's diverticulum (Littre's Henia)
5 clinical types of Hernia :
1) Reducible hernia
It means the hernia can be reduced, either spontaneously when the patient lies down supine, or manually.
For enterocele, the initial part of reduction is difficult. A gurgling sound is usually heard.
For omentocele, the initial part of reduction is easy, but the terminal part is difficult.
2) Irreducible hernia
Usually occurs due to adhesion occurs in between the neck of the sac and contents or even when there's overcrowding of contents.
Other than the irreducibility, there's no other abnormalities.
There's a risk of strangulation at any time.
3) Obstructed hernia
It means the intestinal loop within the hernial sac is obstructed.
Presents with cardinal features of intestinal obstruction.
Eventually progresses towards strangulation.
4) Strangulated hernia
In this case, not only there's bowel obstruction, but with ischaemia of the contents within the sac.
Gangrene of the contents usually occurs 5-6 hours after the onset.
There are 2 types of inguinal hernia :
1) Direct inguinal hernia
It's an accquired hernia.
Almost always seen in elderly, or individuals with the nature of occupation is lifting heavy weights (manual labourers).
Previous apendicectomy, which involves an accidental removal of the ilioinguinal nerve predisposes to direct inguinal hernia, since it weakens the abdominal wall.
The size of hernia is usually small, and rarely descends down to the scrotum.
Since the neck of the hernia is wide, direct inguinal hernia rarely strangulates.
2) Indirect inguinal hernia
Types of indirect inguinal hernia :
1) Bubonocele - The extent of protrusion of the viscus is within the canal
2) Funicular - The processus vaginalis obliterates just above the epididymis. Hence, the hernia is separately palpable from the testis (above it)
3) Complete - extending from the deep inguinal ring, through the canal, exits the superficial ring and down to the scrotum.
Differential diagnosis of inguinal hernia :
a) In males :
1) Vaginal hydrocele
2) Femoral hernia
3) Encysted hydrocele of the cord
4) Lipoma of the cord
5) Undescended testis within the canal
b) In females
1) Femoral hernia
2) Hydrocele of the canal of nuck
Femoral hernia
The incidence of femoral hernia is more common in females (Female:Male ratio=2:1). The major problem regarding femoral hernia the risk of strangulation is high.
This is mainly due to the narrow neck of the hernia sac and rigidity of the femoral ring.
Hence, once femoral hernia is clinically identified, operation must be done as soon as possible.
Differential diagnosis of femoral hernia :
1) Inguinal hernia
2) Saphena Varix
3) Enlarged cloquet's node
4) Femoral aneurysm
5) Psoas abscess
6) Lipoma
History taking in a case of Hernia
1) Firstly, the typical questions for lump
When do you noticed it?
How do you noticed it?
Is there any other lumps in the body?
How does this lump disturbs you? (Associated symptoms)
Any change in the size of the lump since you noticed it?
What is the initial size?
What is the current size?
What do you think is the cause?
2) Questions specific for hernia
Is the swelling reducible?
(If not reducible, ask for previous h/o of reducibility)
When you cough/exerts, does it increase in size?
Any dragging pain, sensation of heaviness?
What's your occupation?
Is there any history of chronically raised intra-abdominal pressure?
(eg, chronic cough, vomiting, abdominal distension, constipation, micturition)
Is there any history of : (Strangulation)
Colicky abdominal pain?
Abdominal distension?
Frequent vomiting?
Absolute constipation?
Is there previous history of abdominal surgery?
Do you smoke? (Increases risk)
*Always bear in mind that hernia in elderly might be a sign of malignancy
Examination of hernia
1) Positioning of patient and exposure
Examine the patient while he/she is standing.
Exposure - umbilicus to the knee
2) Inspection
Note, is it right/left sided or bilateral?
Is it confined to the groin, or it extends down to the scrotum?
What's the shape?
Measure the size of the swelling.
Over the skin of the swelling, is there signs of inflammation?
Ask the patient to look up the ceiling and cough. Does it the swelling expands?
3) Palpation
Check whether there's any rise of temperature
Try getting above the swelling, using your index finger and thumb. If possible, then, most likely it's a pure scrotal lump, otherwise, it's an inguino-scrotal swelling.
Comment on the surface, and note if there's any tenderness.
Is the testis separately palpable from the swelling?
Is the skin over the swelling pinchable?
Now, stand beside the patient.
Place your right hand over the patient's back, with your left hand approximately parallel to the inguinal ligament, place it over the swelling.
Now ask the patient to cough.
Note any increased tension of the contents and any expansile cough impulse.
Now, ask the patient to lie down in supine position.
If the swelling does not reduce spontaneously, ask if he/she can reduce it him/herself.
If not possible, then, manually reduce it yourself.
Note the position of pubic tubercle.
While patient in standing position, gently press over the swelling, and then it's lower part.
Then, gently lift the swelling upwards, and towards the superficial ring.
If the swelling reduces at a point medial and above to the pubic tubercle, it's an inguinal hernia.
If the swelling reduces at a point lateral and below to the pubic tubercle, it's femoral hernia.
Then, try sliding your hand laterally and upwards, towards the deep ring.
Can the swelling be controlled by pressure over the deep ring?
Now, remove your hand from the area of swelling.
For direct hernia, it projects directly forwards.
For indirect hernia, it runs obliquely through the canal, then only protrudes out.
4) Deep ring occlusion test
After complete reduction of hernia, place your thumb over the deep ring.
Ask the patient to cough.
If the swelling doesn't reappears -> Indirect inguinal hernia
If the swelling appears medial to your thumb -> Direct inguinal hernia
5) Auscultation
Any bowel sounds?
6) Examine the abdomen for any signs of raised intra-abdominal pressure
Large bladder?
Enlarged prostate?
Pregnancy?
Ascites
6) Examine the abdomen for any signs of raised intra-abdominal pressure
Large bladder?
Enlarged prostate?
Pregnancy?
Ascites
Subscribe to:
Posts (Atom)